Environmental Science and Engineering
Wastewater monitoring in COVID-19 surveillance
Microbiologist Peiying Hong explains current research into COVID-19 monitoring and surveillance using wastewater.
KAUST researchers are analyzing wastewater for SARS-CoV-2, the virus that causes COVID-19. © 2020 KAUST; Anastasia Serin. /en/article/976/wastewater-monitoring-in-covid-19-surveillance%C2%A0
KAUST researchers are analyzing wastewater for SARS-CoV-2, the virus that causes COVID-19. © 2020 KAUST; Anastasia Serin. /en/article/976/wastewater-monitoring-in-covid-19-surveillance%C2%A0
Several research groups around the world are analyzing wastewater for SARS-CoV-2, the virus that causes COVID-19. Studies show that the virus can be detected in the feces of some infected patients. There is hope that “wastewater-based epidemiology” could hold promise for monitoring COVID-19 outbreaks in communities.
To understand more about the potential of this research, KAUST Discovery spoke with Peiying Hong, an applied environmental microbiologist at KAUST. Hong has conducted years of research monitoring microbial contaminants in wastewater and reclaimed waters, including bacteria, viruses and genes1.
What is the current knowledge about the detection of SARS-CoV-2 in feces and in human wastewater?
SARS-CoV-2 is a respiratory virus like SARS-CoV, the virus that causes SARS, and both can be shed through feces in infected patients. Scientists originally thought that SARS-CoV-2 was only shed in the feces of patients who reported diarrhea, but now it appears that some infected patients, even without diarrhea, could be shedding the virus through their feces into human wastewater. Monitoring municipal wastewater for SARS-CoV-2 can be a useful method for detecting an outbreak.
Peiying Hong and her team have conducted years of research monitoring microbial contaminants, such as bacteria, viruses and genes, in wastewater and reclaimed waters.
© 2020 KAUST
This is especially important if we consider some of the latest statistics. Globally, SARS-CoV-2 has infected more than 68 million people at the time of writing, with approximately 1.5 million reported deaths and 46 million reported to have recovered. Testing as many individuals as possible for SARS-CoV-2 is a key recommendation to contain the spread of the virus. But this is not feasible in some countries due to the burden that this strategy imposes on the local testing system. Hence, monitoring wastewaters for SARS-CoV-2 could become a more time- and cost-effective surveillance strategy.
Researchers from many countries are now looking for this virus in their wastewaters. So far, the studies collectively demonstrate the proof-of-concept, where gene fragments associated with SARS-CoV-2 can be detected in wastewater, particularly in countries with a current outbreak.
But wastewater monitoring for emerging pathogenic viruses is still in its early stages because so much remains unknown. For example, what is the detection sensitivity of the method? How many cases can it detect within a population? What are the decay rates of the virus in wastewater and in the presence of various environmental factors?
Could wastewater surveillance help governments become aware of potential new waves of COVID-19 earlier? How?
It will depend on the definition of “early.” In my opinion, wastewater monitoring seems likely to only be able to detect SARS-CoV-2 when it has already infected a few hundred or even thousands in a community of a few hundred thousand inhabitants. Improvements are needed in the exact detection sensitivity of the method because there are many challenges in monitoring wastewater for a virus such as SARS-CoV-2. For example, any pathogenic virus will be highly diluted in a large volume of wastewater. We will need to recover these viruses from the large volume of wastewater and concentrate them into smaller volumes for analysis.

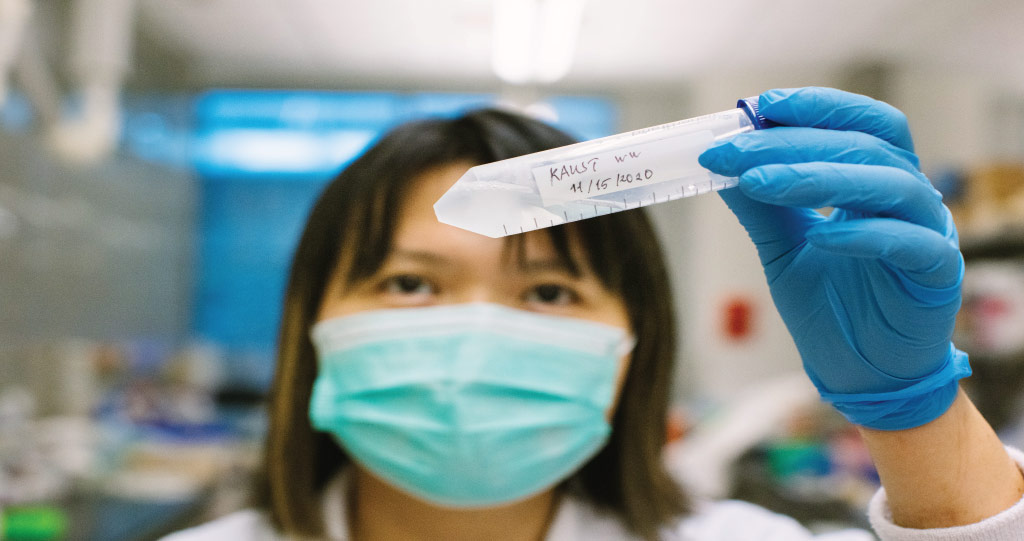
Pathogenic viruses are highly diluted in large volumes of wastewater and natural organic matter and so must be concentrated into smaller volumes for analysis.
© 2020 KAUST
Another problem is that wastewater has high concentrations of natural organic matter, and viruses tend to easily aggregate and adsorb onto particulates, making recovery of viruses difficult. Also, the nature of wastewater means most of the current protocols can only process small volumes of wastewater at a time. This limits the probability of detecting a rare event, say, for instance, if only one person is infected in a community. Most studies analyzing the presence of SARS-CoV-2 in wastewater are based in countries experiencing a widespread outbreak, which is why they have been successful at detecting the virus due to the increased viral load.
Despite these challenges, wastewater monitoring could theoretically assist governments to become aware of new waves. This would require continuous monitoring to establish the baseline abundance of the virus in wastewater, followed by monitoring for any deviations from this baseline that could indicate an incoming wave.
Is there a way to monitor wastewater for future new or unknown viruses?
Most current efforts use “reverse transcription quantitative polymerase chain reaction” (RT-qPCR) to monitor for SARS-CoV-2. This tool can only detect known RNA viruses. To monitor for future new viruses via wastewater, we would need to fulfill at least two criteria. First, the viruses would need to be shed through feces into wastewater. Second, we need to know their genome so that the specific reagents needed for RT-qPCR can be designed. An alternative approach for unknown viruses, whose genomes are not yet known, could use high-throughput sequencing and bioinformatics.

RT-qPCR analysis is currently the gold standard for testing for the presence of SARS-CoV-2.
© 2020 KAUST
Are there any international efforts where governments already employ wastewater surveillance as a strategy for monitoring COVID-19?
Australia and Singapore are working with their local researchers to look for the virus in wastewaters. I am sure there are more countries looking into this as a monitoring tool. However, it is important to emphasize that, currently, wastewater monitoring can only complement the current swab-testing approach because it is not sensitive enough to pick up a small number of cases.
What is the number of positive cases of SARS-CoV-2 for it to be picked up in wastewater such as sewage networks?
Our study2 estimates that in a population of 10,000 people, there would need to be around 253–409 positive cases to be able to detect SARS-CoV-2 RNA in wastewater. However, more research is needed to confirm this number under different circumstances and using different experimental regimes.
To estimate this number for our study, we used the closed community setting of a hospital as a semi-controlled environment so that we could verify, through hospital records of admission and discharge records, the number of patients that were contributing SARS-CoV-2 RNA to the wastewater of the hospital. Located in Jeddah, Saudi Arabia, the hospital is designated to be a COVID-19 treatment hospital, with no visitors allowed, so we knew that the caseload in the water came only from patients (and also potentially asymptomatic staff because those with symptoms were swab tested).
Wastewater was collected from two sites in the hospital, the underground septic tank (1150 cubic meters) and the roof-top aerobic biological tank (750 cubic meters), over six weeks in 2020 from about mid-April to mid-July 2020. We estimated that this volume of water was equivalent to a community of about 2900 people, with each member using about 260 liters per person per day.
This is just an early study, however, which needs to be confirmed through more research. For instance, we would need to look at different sites and also sites in different locations with different sampling regimes, wastewater volumes and a range of other environmental factors. However, this range provides a good “rule of thumb” for monitoring this virus during a pandemic.
More gene fragments of the SARS-CoV-2 virus were found in the septic tank, which suggests that the virus was already degrading in the early stages of the wastewater treatment. This has implications for both the use of wastewater-based epidemiology and the safety of wastewater for those working in close proximity.
If SARS-CoV-2 is appearing in wastewater, what are the risks of being infected for people working in wastewater plants, or even animals where treated wastewater is used for irrigation, for example?
The risks of being infected by treated wastewater are very low. Even in countries experiencing outbreaks, the viral load of SARS-CoV-2 detected in untreated wastewaters is very low, and the multiple barrier treatment technology in most wastewater treatment plants is efficient enough to remove SARS-CoV-2 from wastewater. Also, SARS-CoV-2 does not persist well in the presence of common disinfectants like chlorine, ultraviolet light and sunlight.
People who work in wastewater treatment plants do face a higher risk because they are exposed to contaminants over a longer duration. But it is important to point out that the risks may not only be due to SARS-CoV-2 alone, even though it is on everyone’s mind now, but also from other human enteric pathogenic viruses that may be present in high abundance in untreated wastewaters. This is why they need to engage in best work practices, regularly go through safety training and be equipped with the appropriate personal protective equipment.
What needs to be done to make sure that treated wastewater is safe from SARS-CoV-2? What kinds of technologies are needed? Are these technologies already in use?
The current treatment technologies are already doing a sufficiently good job in mitigating the risk from SARS-CoV-2 because the abundance of this virus in untreated wastewater is quite diluted to start with. Most wastewater treatment plants can achieve at least a 99.999 percent reduction of the virus in the final disinfection step. If treatment plants are not achieving this minimal reduction efficiency, it could be because they are not mandated to perform a final disinfection step, but they should consider doing this now.
Is your team at KAUST undertaking any SARS-CoV-2-related research?
We have been monitoring wastewater generated by our KAUST community since December 2019, before the first case of SARS-CoV-2 was detected in Saudi Arabia. The idea is to continue monitoring so that, as we exit from hibernation and as people return when travel restrictions are lifted, we can compare new data against the baseline to detect deviations from the baseline.

Peiying Hong (right), along with two postdocs in her group, Andri Rachmadi (center) and David Mantilla-Calderon (left), have been monitoring wastewater generated in KAUST since December 2019, before the first case of SARS-CoV-2 was detected in Saudi Arabia.
© 2020 KAUST
We have also been working with collaborators in Jeddah to monitor wastewaters collected from outside KAUST.
In parallel, many colleagues at KAUST are actively contributing their expertise in terms of surveillance, genome sequencing, diagnostics and modeling, to name just a few. This collective effort signifies that KAUST is in solidarity with the rest of the world and is actively contributing in the fight against this virus.
References
- Jumat, M.R., Hasan, N.A., Subramanian, P., Heberling, C., Colwell, R.R. & Hong, P.Y. Membrane bioreactor-based wastewater treatment plant in Saudi Arabia: Reduction of viral diversity, load, and infectious capacity. Water 9, 534 (2017).| article
- Hong, P.Y., Rachmadi, A.T., Mantilla-Calderon, D., Alkahtani, M., Bashawri, Y. M., Al Qarni, H., O’Reilly, K.M. & Zhou, J. (2021). Estimating the minimum number of SARS-CoV-2 infected cases needed to detect viral RNA in wastewater: To what extent of the outbreak can surveillance of wastewater tell us?. Environmental Research 195, 110748. | article
You might also like

Environmental Science and Engineering
Ultrathin water repellent membrane advances desalination
Environmental Science and Engineering
Bacteria reveal hidden powers of electricity transfer

Environmental Science and Engineering
Wastewater surveillance tracks spread of antibiotic resistance

Bioscience
Super fungi survive extreme Mars-like environments

Environmental Science and Engineering
Rethinking food systems to restore degraded lands

Environmental Science and Engineering
Combat climate change by eliminating easy targets

Environmental Science and Engineering
Wastewater treatment to fight the spread of antibiotic resistance

Bioscience