Bioscience
“Sticky” stem cells make for better transplants
Enhancement of adhesion molecules improves the ability of blood-forming stem cells to take root in transplant recipients.
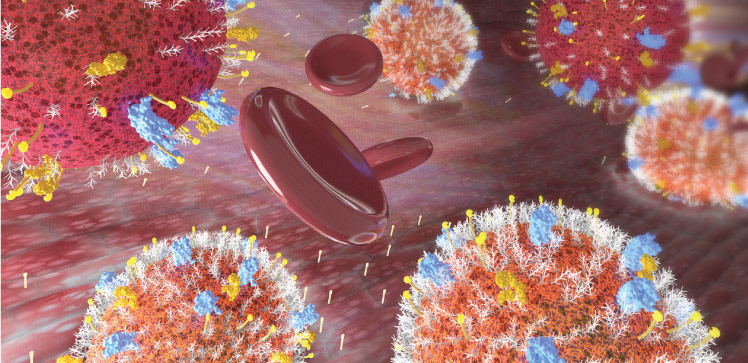
Treatments that boost the “stickiness” of blood-forming stem cells could help improve the success of bone marrow transplants for patients suffering from leukemia and other blood disorders.
A KAUST-led research team identified two such drug treatments that enhance the activity of molecules involved in cell adhesion. Stem cells exposed to these drugs were better able to enter the bloodstream of recipient mice, make their way to the bone marrow and start making new blood.
“This is a crucial finding,” says study author Asma Al-Amoodi, a Ph.D. student in Jasmeen Merzaban’s lab at KAUST. “Such information is indispensable for researchers and clinicians, as it will guide which stem cell populations we select for and which treatments we may use prior to injection in order to increase the success and outcomes of the transplantation process.”
Saudi Arabia was the first Arab state to perform a bone marrow transplant, back in 1984, and now hardly a day goes by without someone in the country receiving an infusion of healthy donor-derived hematopoietic stem cells (HSCs) to replace those lost or damaged by disease. But the types of stem cells contained in such a transplant are not all the same.
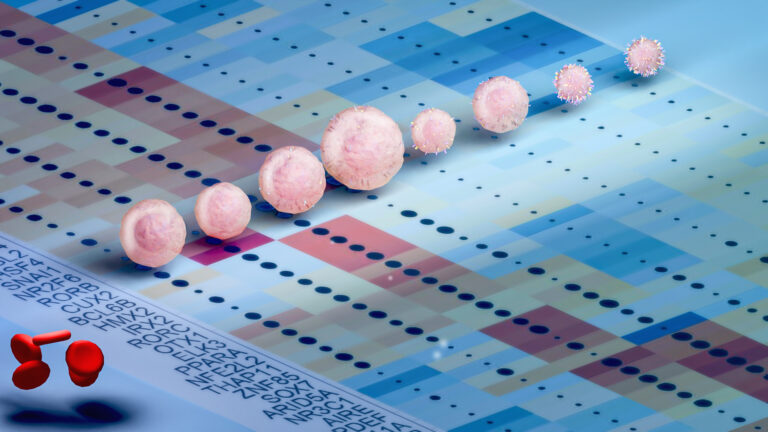
The majority are “short-term” HSCs. These cells can give rise to all manner of white blood cells, thus offering a reprieve from cancer or disease. But the cells have limited capacity for self-renewal, a biological weakness that constrains the duration of their therapeutic benefit.
A different population of rare stem cells has the potential for prolonged reconstitution of the blood-forming system. These “long-term” HSCs can both sustain the stem cell pool and differentiate into their short-term kin, which makes them ideal from a therapeutic standpoint. But long-term HSCs have their own drawback: they are not particularly adept at engraftment, the process of taking root in recipient individuals — and KAUST researchers have now discovered why.
Merzaban and her lab group showed that, compared to short-term HSCs, the reduced expression of key adhesion molecules in long-term HSCs explained their poor engraftment ability. The researchers then found a type of drug commonly used to treat diabetes; when added to long-term HSCs, this drug altered the dynamics of cell surface adhesion molecules in ways that improved uptake of the cells in mice.
Another type of adhesion-targeted treatment also augmented the engraftment potential of short-term HSCs — and, as an added bonus, it made the cells behave more like their long-term counterparts.
Merzaban next hopes to test the strategy with human stem cells and human recipients. “The results of our study suggest that by enhancing the adhesion of these stem cells, we could improve the ability of both types of HSC populations to migrate, engraft and provide functional blood cells to patients,” she says.
References
-
Al-Amoodi, A.S., Li, Y., Al-Ghuneim, A., Allehaibi, H., Isaioglou, I., Esau, L.E., AbuSamra, D.B. & Merzaban, J.S. Refining the migration and engraftment of short-term and long-term HSCs by enhancing homing-specific adhesion mechanisms. Blood Advances 6, 4373–4391 (2022).| article
You might also like

Bioengineering
Bio-inspired network structures for next-generation AI

Bioscience
Robust workflow built for chemical genomic screening
Bioscience
Cell atlas offers clues to how childhood leukemia takes hold
Bioscience
Hidden flexibility in plant communication revealed

Bioscience
Harnessing the unintended epigenetic side effects of genome editing
Bioscience
Mica enables simpler, sharper, and deeper single-particle tracking
Bioengineering
Cancer’s hidden sugar code opens diagnostic opportunities
Bioscience